Agentic AI in Healthcare Diagnosis and Treatment: What It Actually Takes to Deploy It Safely

Healthcare is at an inflection point that cannot be ignored.
The global agentic AI in healthcare market was valued at $538 million in 2024 and is projected to reach nearly $5 billion by 2030 — a 45% compound annual growth rate. That is not a forecast about the distant future. That is infrastructure investment happening right now, at scale, across health systems that have decided waiting is the more expensive option.
The pressure is real on every front. Vention Teams reported that 73% of patients globally have faced delays in care, waiting an average of 70 days for an appointment — and one in three say their health worsened as a result.
At the same time, 35% of clinicians spend more time on paperwork than on direct patient care, while 57% of healthcare organisations identify administrative automation as the single greatest opportunity for AI value creation according to Electroiq. Meanwhile, the workforce gap is widening: nursing vacancies affect 66% of providers, contributing to documentation backlogs and safety events.
AI is already inside the building. Agentic AI is now deployed in 68% of healthcare organisations — making it the third most adopted AI application in the sector. But adoption is not the same as execution. Gartner predicts that over 40% of agentic AI projects will be cancelled by the end of 2027, due to escalating costs, unclear business value, and inadequate risk controls.
The reason most of them fail is not the technology. It is the foundation — fragmented data, absent governance, and execution logic bolted onto systems that were never designed to act autonomously.
The organisations that will win are not the ones that deploy AI fastest. They are the ones that deploy it correctly — on complete clinical context, with deterministic governance, and with the infrastructure to execute across integrated systems safely.
Gartner projects that by 2028, at least 15% of day-to-day work decisions will be made autonomously through agentic AI, up from virtually zero in 2024. In healthcare, the decisions that cross that threshold will affect patients. That raises the stakes for getting the architecture right to an entirely different level.
This article examines what that architecture actually requires — and the real-world deployment patterns that prove it works.
What Is Agentic AI in Healthcare?
Agentic AI is a class of autonomous, governed systems that can complete multi-step tasks independently, across multiple systems, using reasoning and real-world data. In the healthcare context, that means an AI system capable of:
- Ingesting and reasoning over clinical data from multiple sources simultaneously
- Detecting a relevant signal — a diagnostic anomaly, a staffing gap, a compliance trigger
- Deciding on an appropriate action based on encoded clinical and operational rules
- Executing that action across integrated systems, with or without human approval depending on thresholds
- Logging every step with policy citations, audit trails, and explainability
The critical distinction is between an AI copilot and an autonomous clinical agent. A copilot surfaces a recommendation and waits. An agentic system closes the loop — it moves from insight to action without a human bottleneck at every stage.
The maturity model for enterprise AI reflects this progression clearly:
- Level 1 – Descriptive: What happened? (Static reports)
- Level 2 – Diagnostic: Why did it happen? (BI dashboards)
- Level 3 – Predictive: What will happen? (Forecasting models)
- Level 4 – Prescriptive: What should we do? (Recommendations, AI copilots)
- Level 5 – Agentic: Handle this. (Autonomous, governed execution)
Most healthcare organisations today are stuck between Level 3 and Level 4. The infrastructure gap between prescriptive AI and agentic AI is not a small software upgrade. It requires a fundamentally different approach to data architecture, governance, and execution logic.
Why Traditional AI Fails in Healthcare Diagnosis and Treatment

The core failure of most healthcare AI deployments can be expressed in a single statistic: only 10–20% of healthcare data lives in structured systems. EHR tables, billing codes, transaction logs — these are what conventional BI tools and most AI models can see and reason over.
The other 80–90% of clinical context lives in formats that structured systems cannot parse:
- Radiology reports in PDF format
- Physician consultation notes
- Discharge summaries
- Insurance correspondence and claim attachments
- Lab result attachments and imaging metadata
- Internal emails with negotiated care exceptions
- Compliance documentation and policy files
This is not a data quality problem. It is a data architecture problem. The information is there. The clinical truth is captured. But agents acting on 20% of the available context are not making informed decisions — they are making dangerous half-decisions, at machine speed.
Consider the analogy from financial services: a payment automation agent was deployed with access to ERP data, invoice amounts, and due dates. What it could not see were contract PDFs with negotiated discounts, email threads flagging cash flow concerns, and Slack messages with approval flags. The agent processed every invoice it could see — correctly, by its own logic — and triggered significant overpayments before a human caught the pattern.
Translate that into a clinical environment. An agent that can see structured lab values but not the physician notes flagging a drug interaction. An agent that processes referral routing based on EHR fields but cannot read the discharge summary indicating a contraindication. An agent with a confidence score of 95% — on 20% of the data.
An agent acting on partial context is not an asset. It is a liability with an autonomous execution loop.
This is the foundational problem that any serious implementation of agentic AI in healthcare must solve before anything else.
The Enterprise Data Reality in Healthcare
To understand why this problem persists, it helps to map the data landscape in a typical healthcare organisation.
Structured data — ERP, CRM, POS, transaction systems — accounts for roughly 10–20% of total data volume. Semi-structured data — logs, APIs, event streams — adds another 5–10%. Unstructured data — documents, emails, imaging reports, clinical notes — makes up 70–85% of everything the organisation generates.
BI tools and most AI platforms are built primarily for the structured tier. They are optimised for relational schemas, SQL queries, and dashboard visualisation. They excel at answering the question of what happened. They cannot answer why or what to do next without access to the full data picture.
The implication for healthcare is stark. A patient's medical record in a structured EHR captures coded diagnoses, procedure codes, medication lists, and appointment dates. It does not capture the nuance in a physician's handwritten note, the clinical reasoning in a radiology narrative, or the prior history embedded in a PDF referral letter from another provider. A system that cannot fuse all of these into a unified semantic layer cannot be trusted to make autonomous clinical decisions.
The shift that agentic AI requires — and that next-generation platforms are built to deliver — is from structured data access to unified context across all data types, fused into a single reasoning layer that agents can act on with full situational awareness.
Types of AI Agents in Healthcare
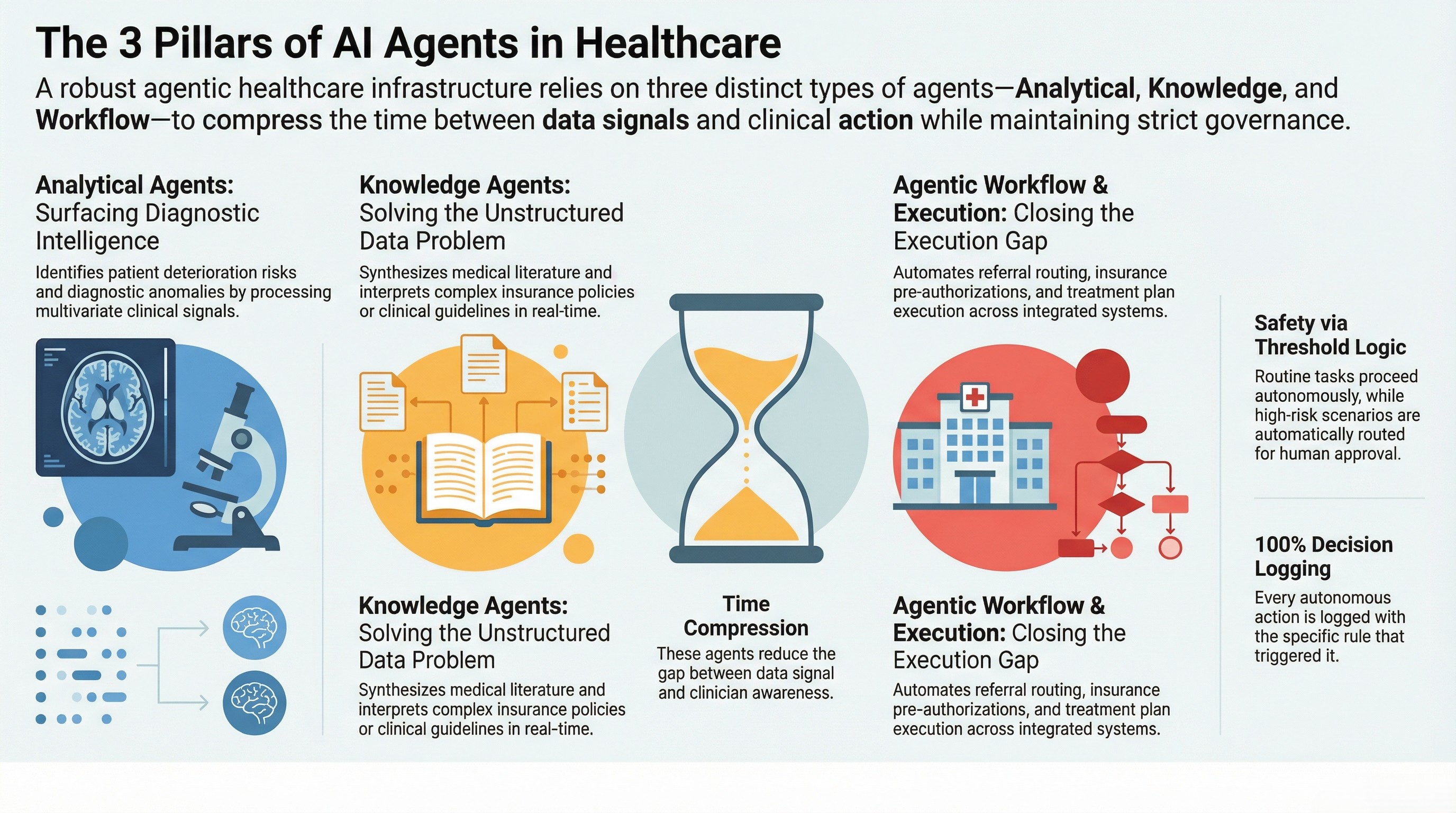
Not all clinical agents serve the same function. A robust agentic healthcare infrastructure typically comprises three categories of agent, each addressing a distinct layer of the clinical and operational workflow.
Analytical Agents
Analytical agents operate on data signals — structured, semi-structured, and fused unstructured sources — to produce diagnostic intelligence. In healthcare, this means:
- Risk prediction: Identifying patient populations at elevated risk of deterioration, readmission, or adverse events based on multivariate clinical signals
- Diagnostic support: Correlating lab results, vital signs, imaging outputs, and clinical notes to surface anomaly patterns that warrant escalation
- Outcome forecasting: Projecting clinical pathways based on intervention history, comorbidities, and population-level benchmarks
Analytical agents do not replace clinical judgment. They compress the time between signal and awareness — surfacing what matters, when it matters, rather than waiting for a clinician to notice a trend buried in a dashboard.
Knowledge Agents
Knowledge agents are designed to read, extract, and reason over documents, literature, and policy frameworks. In clinical settings, this includes:
- Medical literature synthesis: Retrieving and summarising relevant clinical research in the context of a specific patient case or treatment decision
- Guideline referencing: Accessing and interpreting national clinical guidelines, formulary restrictions, or institutional protocols in real time
- Compliance interpretation: Parsing insurance policy documents, prior authorisation requirements, and regulatory documentation to identify applicable rules
Knowledge agents address the unstructured data problem directly. They can read PDFs, process clinical correspondence, and extract structured meaning from documents that conventional systems cannot touch.
Agentic Workflow Agents
Agentic workflow agents close the execution gap. They do not just surface insight — they act on it, across integrated systems, with governance controls that define where human approval is required and where the agent can proceed autonomously. In healthcare, this covers:
- Referral routing: Classifying incoming referrals, matching to appropriate specialists, and initiating scheduling workflows without manual triage
- Insurance pre-authorisation: Pulling clinical documentation, interpreting policy requirements, and submitting prior authorisation requests automatically
- Treatment plan execution: Triggering order sets, scheduling follow-ups, and coordinating care team notifications based on clinical decision logic
- Medication workflow management: Processing refill requests, flagging drug interactions from unstructured notes, and routing high-risk approvals to a clinician
The governance layer is what separates safe agentic execution from reckless automation. A well-designed clinical workflow agent operates on threshold logic: a routine prescription refill below a defined risk score proceeds autonomously; a controlled substance request or complex polypharmacy scenario routes to a pharmacist or physician for approval. Every decision — including autonomous ones — is logged with the rule that triggered it.
Agentic AI in Healthcare Diagnosis: Real Workflow Patterns
Agentic AI in Radiology
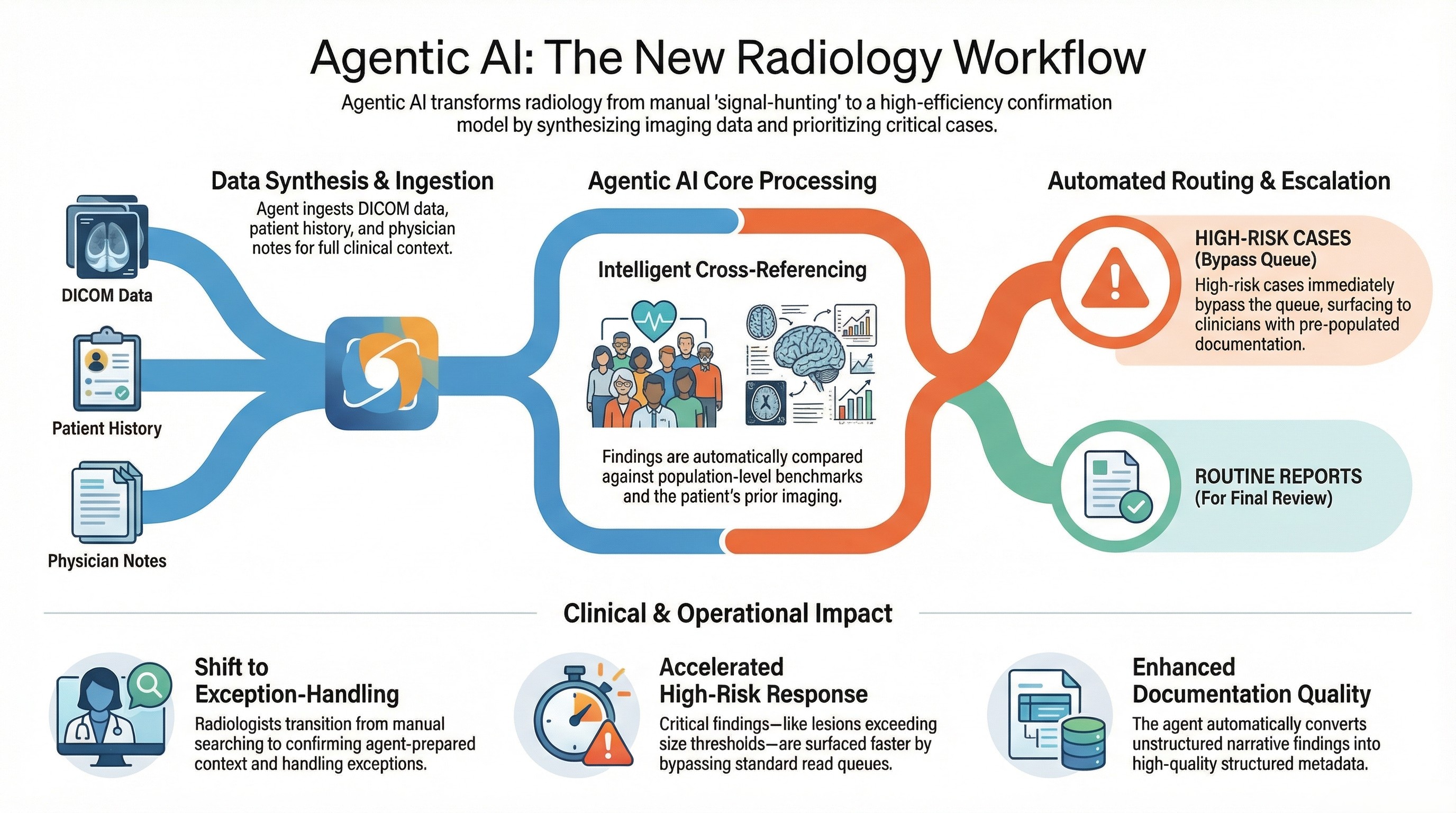
Radiology is one of the highest-value and highest-volume applications for agentic AI in clinical diagnosis. The workflow pattern is well-suited to agentic architecture because the inputs are consistent, the outputs are high-stakes, and the volume of cases far exceeds what radiologist capacity can handle without AI augmentation.
An agentic radiology workflow operates as follows:
An imaging study is completed. The agent ingests the DICOM image data and any associated metadata. It retrieves the patient's prior imaging history, correlating findings across time. It accesses the referring physician's notes from the patient's clinical record — including unstructured narrative — to understand the clinical question being asked. It processes the radiologist's preliminary report draft, cross-referencing findings against population-level benchmarks and known risk indicators.
Where findings exceed a defined threshold — a lesion above a certain size, a pattern matching a high-risk classification, a discrepancy between current and prior imaging — the agent escalates immediately. It does not wait for a radiologist to complete the read queue. It surfaces the case, prepopulates the escalation documentation, and routes it to the appropriate clinician with full supporting context.
Where findings are routine and below escalation thresholds, the agent completes its correlation work, appends structured metadata to the report, and marks the study for standard workflow. The radiologist reviews, not from scratch, but with agent-prepared context already populated.
The result is a shift in the radiologist's role — from manual signal-hunting to confirmation and exception-handling. Case throughput increases. High-risk cases are surfaced faster. Documentation quality improves because unstructured findings are captured and structured by the agent, not reconstructed manually.
Agentic AI in Clinical Data Management
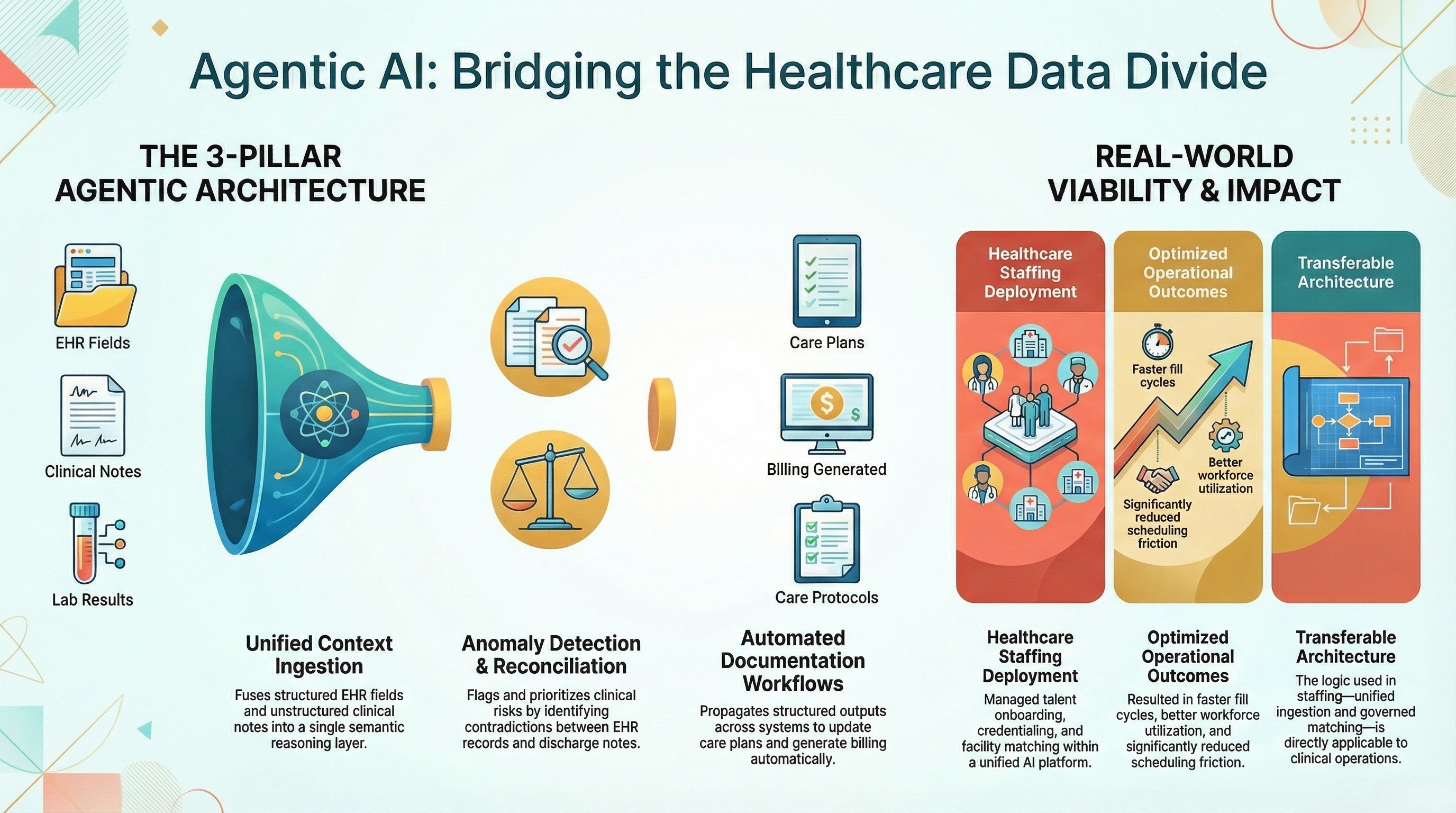
Clinical data management is one of the most operationally burdensome functions in healthcare delivery. Patient records are fragmented across EHR systems, lab portals, imaging archives, referral correspondence, and insurance documentation. Reconciling this data for care coordination, billing, and compliance is almost entirely manual at most organisations.
An agentic data management layer addresses this at the infrastructure level. The architecture requires three capabilities working in concert:
Unified context ingestion: The agent must be able to pull from structured sources (EHR fields, billing codes, lab values), semi-structured sources (HL7 messages, API feeds, appointment event logs), and unstructured sources (clinical notes, discharge summaries, referral PDFs). These cannot exist in separate silos — they must be fused into a single semantic layer where the agent can reason across all of them simultaneously.
Anomaly detection and reconciliation: Once the unified context exists, the agent monitors for inconsistencies — a medication listed in the EHR that contradicts a contraindication flagged in a discharge note, a lab value that was entered in one system but not reconciled in another, a billing code that does not match the documented diagnosis. These anomalies are flagged, prioritised by clinical risk, and routed for resolution.
Automated documentation workflows: Rather than requiring a clinician to manually update multiple systems after each patient encounter, the agent can propagate structured outputs from one system to others — updating the care plan, generating billing documentation, and notifying the care team — based on the encounter notes and clinical decision logic.
Real-world deployments in healthcare-adjacent staffing contexts have demonstrated the architecture's viability. In one implementation, an AI platform was deployed to manage the full talent onboarding and scheduling workflow for a healthcare staffing operation — capturing credentials, matching nursing professionals to facility needs, managing scheduling notifications, tracking compliance requirements, and generating fill-rate reporting.
The result was faster fill cycles, better workforce utilisation, and significantly reduced scheduling friction. The architecture that made this possible — unified data ingestion, governed matching logic, automated notification workflows, and reporting dashboards — is directly transferable to clinical operations management.
Agentic AI in Treatment Execution
The most consequential — and most carefully governed — application of agentic AI in healthcare is treatment execution. This is where the stakes are highest and the governance requirements are most demanding.
Treatment execution agents do not make clinical decisions unilaterally. They operate within explicit rule frameworks that define the boundary between autonomous action and human-required approval. The threshold logic is the governance mechanism, and it must be designed with the same rigour as a clinical protocol.
Medication approval workflows are a practical starting point. A routine refill request for a stable chronic condition, from a patient with no recent changes in their clinical record, can be processed autonomously — the agent retrieves the prescription history, checks for contraindications in the unified clinical context, confirms the prescribing physician is still active, and routes the refill for dispensing. A new prescription for a high-risk medication, or a refill with a recent hospital admission in the patient's record, routes to a physician for review. The agent prepopulates the review with all relevant context — it does not just flag the case, it presents the case.
Oncology treatment pathway orchestration illustrates the more complex end of the spectrum. A treatment protocol involves coordinated scheduling across multiple departments — oncology, radiology, pharmacy, laboratory — with timing constraints, drug ordering sequences, and monitoring requirements that span weeks or months. An agentic system can hold the entire protocol in context, initiate each step at the appropriate time, flag deviations from the protocol, and surface the patient's current clinical status against expected trajectory. Every step is logged. Every deviation triggers a governed escalation. The oncologist remains in the loop at defined decision points — they are not replaced, they are freed from the coordination burden.
Remote monitoring and automatic intervention triggers represent the emerging frontier. Continuous monitoring devices generate patient data in real time. An agentic system can monitor these streams, compare values against individualised thresholds defined in the patient's care plan, and trigger a care team notification when a threshold is exceeded — not on a reporting cycle, but in the moment. For post-operative patients, for chronic disease management, for home-based care programmes, this closes a critical gap in the care continuum.
The governance architecture for treatment execution agents must include complete audit trails, policy-cited decision logs, and clear human-in-the-loop thresholds. Every autonomous action the agent takes must be reviewable, every rule that triggered it must be documented, and every exception must be escalated through a defined pathway. This is not optional — in clinical settings, it is the difference between a system that a hospital can deploy in good conscience and one that creates medico-legal exposure.
Agentic AI in Drug Discovery
Drug discovery represents one of the most data-intensive, documentation-heavy, and time-sensitive research workflows in any industry. The combination of scientific literature, clinical trial data, regulatory documentation, and proprietary research generates exactly the kind of multi-source, high-volume, mixed-format data environment where agentic AI delivers its highest value.
Literature synthesis agents can continuously monitor published research — journals, preprint servers, regulatory submissions — and synthesise findings relevant to an active discovery programme. Rather than research teams manually reviewing thousands of papers per quarter, an agent identifies and extracts the relevant findings, maps them against the programme's existing hypotheses, and surfaces contradictions or supporting evidence in a structured format.
Trial data anomaly detection addresses the integrity challenges of running multi-site clinical trials. Data quality inconsistencies — protocol deviations, data entry errors, patient eligibility flags — are monitored continuously by the agent, surfaced in real time, and routed for investigation before they compound into audit findings.
Protocol compliance monitoring ensures that trial operations adhere to the approved protocol, ICH-GCP requirements, and regulatory submission standards. An agent can track each site's activity against the approved protocol timeline, flag deviations, and generate the documentation required for regulatory response — compressing timelines that previously required weeks of manual preparation.
Regulatory documentation automation applies knowledge agents to the vast documentation burden of drug development. Clinical study reports, safety narratives, submission-ready summary documents — these can be substantially pre-populated from underlying study data and literature synthesis, with human review focused on validation rather than construction.
The architecture required for this is identical to the clinical data management architecture: unified ingestion of structured and unstructured data, semantic governance over the reasoning layer, and an active orchestrator that executes across the research management systems where the work actually happens.
Real-World Case-Based Architecture Patterns
The following architecture patterns are derived from real deployments. Client names are not included — what matters here is the infrastructure logic that delivered results.
Case Pattern 1: Autonomous Clinical Operations Agent
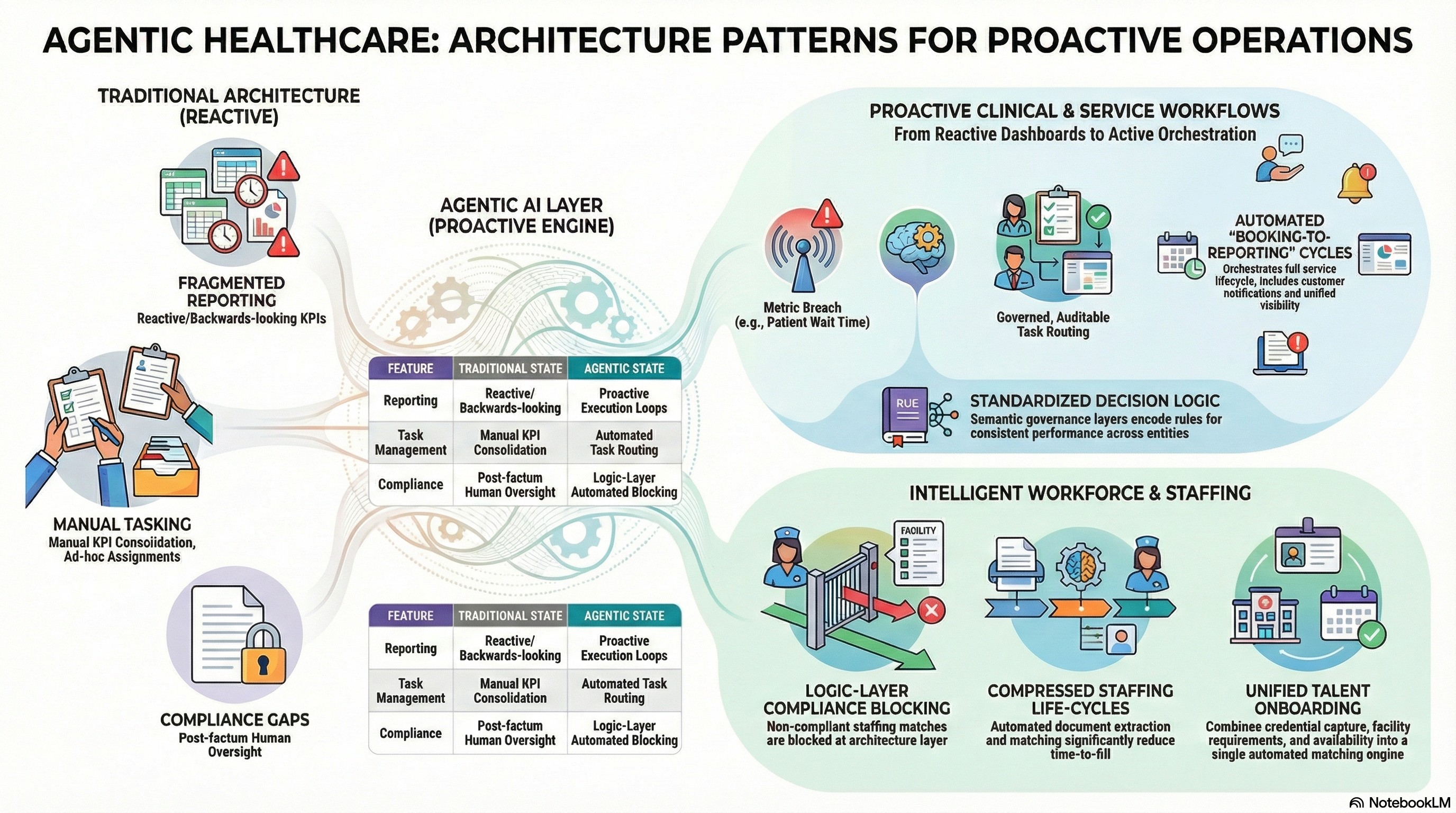
A healthcare services organisation deployed an agentic analytics layer across its multi-entity operations to move from reactive reporting to proactive operational execution. The prior state was fragmented dashboards, manual KPI consolidation, and a reporting cycle that meant leadership was always looking backwards.
The deployed architecture included a unified context engine that standardised operational KPIs across entities, a semantic governance layer that encoded the rules for what constituted a performance exception, and an active orchestrator that translated dashboard insights into governed, auditable actions and tasks. When a metric breached a defined threshold, the agent did not just update a dashboard — it created a task, routed it to the appropriate team, and tracked its resolution.
The results were a shift from reactive reporting to proactive execution loops, standardised decision logic across teams, and automated task creation and completion tracking that reduced the manual overhead of operational management significantly.
Case Pattern 2: Healthcare Staffing Intelligence Agent
A healthcare staffing platform — connecting nursing professionals with healthcare facilities for flexible shifts — deployed an end-to-end agentic platform covering the full staffing lifecycle.
The architecture addressed talent onboarding and credential capture through automated document extraction, matching and scheduling through governed logic that factored facility requirements, nurse credentials, availability, and compliance status, and notification and compliance workflows that reduced manual coordination. Reporting covered fill-rate analytics, utilisation tracking, and variance explanation to facility and platform leadership.
The outcomes included faster fill cycles, better workforce utilisation, and improved staffing responsiveness — the platform could match and deploy qualified staff in significantly compressed timescales compared to manual processes. The credential compliance layer meant that non-compliant matches were blocked at the logic layer, not caught after the fact.
This pattern is directly relevant to clinical workforce management within health systems — the same architecture applies to internal float pools, locum management, and multi-site care delivery coordination.
Case Pattern 3: Healthcare Service Workflow Automation
A UK-based private healthcare and testing provider with high-volume consumer workflows deployed an agentic platform covering the full service delivery cycle — from booking through processing to reporting and analytics.
The prior state required significant manual coordination across booking, processing, and reporting, with status monitoring handled through human oversight and customer communication managed manually. The agentic deployment introduced booking and workflow orchestration that automated the full cycle, status monitoring with automated customer notifications, and unified reporting dashboards covering both operational and analytics views.
The results included more scalable operations with reduced manual overhead, faster customer communications with fewer missed handoffs, and improved service visibility through unified reporting. The architecture demonstrated that even in regulated healthcare environments, the full booking-to-reporting workflow can be governed, automated, and audited end-to-end.
Next-Generation Agentic AI for Transforming Healthcare
What separates infrastructure-grade agentic AI from point solutions is the depth and integration of three architectural layers. Healthcare executives evaluating agentic platforms should assess each.
Tier 1: Unified Context Engine
The unified context engine solves the 80% blind spot. It fuses structured data from EHR and clinical systems, semi-structured data from HL7 feeds and event logs, unstructured data from clinical notes, imaging reports, and correspondence, and external data from clinical guidelines, drug databases, and regulatory sources.
Critically, this fusion produces a single semantic layer — not a data lake that agents query separately. The agent reasons over a unified representation of the patient, the case, and the operational context simultaneously. This is the only architecture that makes clinical agentic decisions safe.
In clinical terms: the agent that processes a medication approval can see the structured prescription history, the unstructured physician notes flagging a drug interaction, the prior imaging report documenting a relevant comorbidity, and the insurance policy document governing the approval requirement — all at once, in the same reasoning context.
Tier 2: Semantic Governance Layer
The semantic governance layer is what makes agentic AI deployable in clinical settings. It encodes the business and clinical rules that govern every decision the agent makes — not as probabilistic suggestions, but as deterministic logic.
This layer holds approval hierarchies, compliance thresholds, clinical decision trees, and escalation policies. It defines, precisely, which actions the agent can take autonomously and which require human approval. Every decision the agent makes is traced to the specific rule that justified it — making every output auditable, defensible, and explainable.
In a HIPAA-governed environment, this layer also holds the privacy and data handling rules that govern what data can be used, retained, or disclosed for each workflow type. The governance layer is not a bolt-on — it is foundational.
Tier 3: Active Orchestrator
The active orchestrator closes the execution gap. It is the layer that connects the agent's reasoning to the systems where clinical and operational work actually happens — EHR platforms, scheduling systems, pharmacy management, CRM, billing engines, compliance reporting tools.
It executes multi-step workflows across these systems, manages human-in-the-loop touchpoints according to the governance layer's thresholds, and tracks the completion and outcome of every action. It is not a scripted automation — it handles exceptions, adapts to system responses, and escalates appropriately when a workflow cannot complete as planned.
The combination of these three layers — unified context, semantic governance, active orchestration — is what transforms AI from an insights tool into an execution infrastructure.
Agentic AI Healthcare Startups vs Enterprise-Grade Infrastructure
The agentic AI healthcare market includes a growing number of point solutions — diagnostic AI tools, administrative automation products, clinical documentation assistants. These are not without value, but they represent a fundamentally different architecture than enterprise-grade agentic infrastructure.
Point solutions typically offer a narrow, well-defined capability: a model that reads radiology images, a tool that drafts prior authorisation letters, an assistant that summarises clinical notes. Each solves a discrete problem. None of them close the execution loop across the full clinical workflow.
The limitations become apparent in production. A radiology AI that surfaces a finding cannot route it to the correct specialist and initiate the scheduling workflow. A prior authorisation tool that drafts a letter cannot submit it, track its status, and escalate if rejected. A documentation assistant that summarises notes cannot propagate those summaries into the systems where care coordination happens.
Enterprise-grade agentic infrastructure addresses the full loop: context fusion across all data types, semantic governance that encodes clinical and operational rules, and active orchestration that executes across the integrated system landscape. The difference is not a matter of scale — it is a matter of architecture.
Security and compliance requirements further differentiate enterprise-grade platforms. Deployments in clinical environments require SOC 2 Type II certification, ISO 27001 alignment, GDPR compliance where applicable, AES-256 encryption with TLS 1.3, and full audit logs with rule citations. Data governance must ensure that patient data is never used to train models without explicit authorisation, and that data residency requirements are met for each deployment context. These are not features — they are prerequisites for clinical deployment.
Autonomy requires trust. Trust requires control. Enterprise-grade governance infrastructure is the only architecture that earns both.
How to Evaluate Agentic AI Readiness in Healthcare
Before deploying agentic AI in clinical settings, healthcare organisations should assess their current state against several infrastructure dimensions.
Data architecture: Can your organisation access and fuse structured EHR data, unstructured clinical notes, and semi-structured event logs in a single reasoning context? If your AI tools can only see your EHR fields, you are operating with the 20% of context that creates the liability problem.
Governance maturity: Do you have documented, machine-readable clinical and operational rules that could govern an agent's decision logic? The governance layer must exist before an agent can be deployed safely — it cannot be retrofitted.
System integration: Is your technology landscape integration-ready? Agentic orchestration requires the ability to execute actions in EHR systems, scheduling platforms, pharmacy systems, and billing engines. If these systems are not accessible via APIs or integration layers, the execution capability cannot be activated.
Audit and compliance readiness: Can your current systems produce a decision audit trail that explains, for any given agent action, what data was used, what rule was applied, and what the outcome was? In clinical settings, this is not optional — it is the compliance standard.
Organisations that score well across these dimensions are ready to deploy agentic infrastructure and capture the efficiency, quality, and speed gains that early adopters are already realising. Organisations with gaps in data architecture or governance maturity should address those foundations before layering autonomous execution on top.
The Future of Agentic Healthcare
The trajectory of agentic AI in healthcare points toward a fundamental restructuring of clinical operations. Not the replacement of clinicians — but the elimination of the operational overhead that consumes clinical capacity and delays care delivery.
In the near term, the gains are measurable and achievable: faster diagnostic triage, reduced prior authorisation delays, automated documentation, more responsive care coordination, and real-time workforce management. These are operational improvements with direct patient impact.
In the medium term, the architecture enables something more significant: continuous, autonomous monitoring of patient populations at scale. Not periodic check-ins, not reactive responses to deterioration — but agents that maintain awareness of every patient in a care programme, surface deviations from expected trajectory in real time, and initiate the appropriate care response without waiting for a scheduled review.
In the longer term, the enterprise evolution model — from Reporting to BI Dashboards to Conversational Analytics to Agentic Execution — will be complete in healthcare. The question clinical leaders will be asking will not be "should we automate this workflow?" but "what is our threshold model for autonomous execution, and how do we govern it?"
That question requires infrastructure thinking, not tool selection. The organisations that invest now in unified context engines, semantic governance layers, and active orchestration will be the ones positioned to answer it — and to deliver the care quality improvements and operational efficiencies that autonomous clinical execution makes possible.
Ready to Move from Clinical Insight to Clinical Execution?
Most healthcare organisations already have the data. What they lack is the infrastructure to act on it — governed, auditably, at speed. If you're evaluating what it would take to move your clinical or operational workflows from reactive dashboards to autonomous execution, Assistents AI is built specifically for that transition.
It is not a diagnostic tool or a chatbot — it is the context engine, governance layer, and orchestration infrastructure that makes agents safe enough to deploy in production environments where the stakes are real.
If that is the problem you are trying to solve, it is worth a conversation.
Frequently Asked Questions
What is agentic AI in healthcare diagnosis and treatment?
Agentic AI in healthcare is an autonomous, governed system that can detect clinical signals, decide on appropriate actions based on encoded rules, execute workflows across integrated clinical systems, and log every decision with full auditability. It differs from conventional healthcare AI in that it closes the loop between insight and action — it does not just surface recommendations, it executes them, within defined governance boundaries.
How is agentic AI different from traditional healthcare AI?
Traditional healthcare AI — diagnostic models, BI dashboards, predictive analytics — produces insight and stops there. A human must interpret the output and decide what to do. Agentic AI continues past insight to execution: it decides, acts, routes approvals, coordinates across systems, and tracks outcomes. The governance layer defines where autonomous action is permitted and where human approval is required, making the autonomy controllable and auditable.
Is agentic AI safe for clinical decision-making?
Safety in agentic AI depends entirely on the governance architecture. A system with a unified context engine that prevents decisions on partial data, a semantic governance layer that encodes clinical rules and escalation policies, and complete audit trails with policy-cited decision logs can be deployed safely in clinical settings. A system without these layers — acting on incomplete data with no deterministic governance — is not safe, regardless of its diagnostic accuracy on benchmarks.
What are examples of agentic AI in healthcare?
Real-world applications include agentic radiology workflows that auto-triage high-risk scans and pre-populate escalation documentation; healthcare staffing platforms that autonomously match, schedule, and manage compliance for clinical workforce deployment; prior authorisation automation that retrieves, assembles, and submits documentation without manual coordination; and clinical data management agents that reconcile records across EHR, lab, and imaging systems in real time.
How does agentic AI improve radiology workflows?
An agentic radiology system ingests imaging data, retrieves prior history, accesses referring physician notes from the clinical record, and cross-references findings against risk thresholds — all before the radiologist begins their review. High-risk cases are surfaced and escalated immediately. Routine cases arrive with context pre-populated. The radiologist's role shifts from signal-hunting to confirmation and exception handling, improving throughput and reducing the time from imaging to clinical decision.
Can agentic AI manage clinical data autonomously?
Yes, within a governed architecture. An agentic clinical data management system can ingest data from structured, semi-structured, and unstructured sources, detect anomalies and reconciliation gaps, propagate structured outputs across integrated systems, and generate documentation for billing and compliance — all autonomously, with human review triggered only when exceptions exceed defined thresholds. The governance layer defines what the agent can do independently and what requires human validation.

Transform Your Business With Agentic Automation
Agentic automation is the rising star posied to overtake RPA and bring about a new wave of intelligent automation. Explore the core concepts of agentic automation, how it works, real-life examples and strategies for a successful implementation in this ebook.
More insights
Discover the latest trends, best practices, and expert opinions that can reshape your perspective
Contact us









.jpg)


