AI Agents in Healthcare Administration: From Patient Onboarding to Claims

According to the National Academy of Medicine's 2024 report, administrative costs reached $280 billion annually (Source: NAM Action Collaborative, 2024-11-15). Over the past two years, about 65% of healthcare leaders have said that handling insurance claims has become even more complicated.
On average, hospitals spend around 25% of their income just on administrative tasks. At the same time, patients often wait up to 45 minutes just to complete basic onboarding forms.
Take Metro General Hospital, for example. Their chief operating officer recently took a close look at the hospital's revenue cycle and found some troubling issues.
Even with 300 people working in administrative roles, the hospital still faced a 12.3% claims denial rate. That mistake alone cost the 400-bed hospital $3.2 million in lost income.
On top of that, patient complaints about long check-in times went up by 35%, and nurses said they now spend nearly half their time filling out forms instead of helping patients. In this blog, let us understand AI agents in healthcare administration in depth.
What are AI Agents in Healthcare? (Definition + Core Functions)
Healthcare AI agents are rapidly transforming the way the healthcare industry operates, bringing a new level of intelligence and efficiency to both clinical and administrative workflows.
These advanced digital assistants harness the power of large language models, natural language processing, and machine learning to automate routine tasks, support clinical decision making, and deliver personalized care to patients.
By seamlessly integrating with electronic health records, healthcare AI agents can analyze vast amounts of patient data—including medical history, lab results, and relevant medical research—in real time.
This enables healthcare professionals to generate personalized treatment plans tailored to each patient’s unique needs, predict patient outcomes, and make more informed clinical decisions. The result is not only improved patient care, but also a significant reduction in administrative burdens that have long challenged healthcare organizations.
AI agents can interpret natural language requests from both patients and staff, making it easier to access information, schedule appointments, and facilitate accurate reimbursement.
As the healthcare industry continues to evolve, these intelligent systems are poised to play a vital role in enhancing health outcomes, streamlining operations, and ensuring that healthcare professionals can focus on what matters most: delivering high quality patient care.
Why Hospitals Bleed Money on Manual Workflows?
Traditional healthcare workflows create cascading inefficiencies that compound throughout the revenue cycle. Insurance verification alone requires an average of 20 minutes per patient, with staff manually checking eligibility across multiple systems.
This process involves duplicate data entry across six or more platforms, resulting in a 30% error rate in patient information capture.
The complexity multiplies during claims processing, where hospitals face a 9.5% average denial rate according to the Healthcare Financial Management Association's 2024 research. And, in 2025, the denial rates continue to climb. (claims denial rate 2025)
Nearly 48% of these denials require manual review and rework, extending the average reimbursement cycle to 14 days. For a typical 200-bed hospital processing 15,000 claims monthly, this translates to 1,425 denied claims requiring costly manual intervention.
Pro Tip: Track your "administrative touch time" per patient encounter. Most hospitals discover that 60-70% of this time involves repetitive data validation tasks that AI agents can handle automatically.
Current Patient Onboarding Pain Points
Patient registration represents the first and most critical touchpoint in the healthcare revenue cycle. Traditional onboarding requires patients to complete multiple forms, often duplicating information already available in their insurance records or previous visits.
Staff must then verify this information across separate systems, creating bottlenecks that extend wait times and frustrate both patients and caregivers.
Insurance verification delays average 20 minutes per patient, with complex cases requiring up to 45 minutes of staff time. Pre-authorization requests for specialized procedures add another layer of complexity, often requiring multiple phone calls and fax submissions.
This manual approach creates a patient experience that resembles navigating bureaucracy rather than receiving healthcare.
The financial impact is substantial. Each minute of extended onboarding time costs hospitals approximately $2.30 in staff wages and overhead, while patient satisfaction scores decrease by 0.3 points for every 10-minute delay beyond expected wait times.
Claims Processing Bottlenecks
Claims processing represents the culmination of healthcare administration complexity. Medical coding accuracy depends heavily on manual review, with even experienced coders achieving only 85-90% accuracy rates on complex cases.
Prior authorization requirements vary significantly across insurance providers, creating inconsistent workflows that staff must navigate differently for each patient.
The 9.5% average claims denial rate masks significant variation across procedure types and insurance providers. Surgical claims experience denial rates up to 15%, while routine office visits average 4-6% denials.
Medicare claims typically process more smoothly than commercial insurance claims, which require extensive documentation and pre-authorization validation.
2025 Administrative Cost Trends & Benchmarks
AI agents in healthcare administration is growing fast, and by 2025, many changes will happen that most people don’t know much about:
- Behind-the-scenes help: AI will not just help with big surgeries or diagnosis. It will also quietly manage hospital tasks like checking if insurance is approved, sending reminders for medicines, or arranging test reports for doctors. Most people won’t even notice, but it will make things faster and more organized.
- AI for second opinions: AI will be used as a smart assistant to give doctors extra suggestions. For example, if a doctor misses something in a report, AI might catch it. This doesn’t replace doctors, but helps them reduce mistakes.
- Spotting health problems early: AI tools will soon read your health records and tell doctors what might go wrong even before symptoms start. This could help stop diseases like kidney failure or stroke from getting worse.
- Less paperwork, more care: With AI handling the boring work, doctors can spend more time talking to patients.
How AI Agents Orchestrate Seamless Healthcare Workflows?
AI agents in healthcare administration operate as intelligent orchestrators, coordinating multiple administrative tasks simultaneously while learning from each interaction to improve performance.
Unlike traditional robotic process automation (RPA) that follows rigid scripts, AI agents adapt to variations in patient data, insurance requirements, and clinical scenarios.
These systems integrate directly with existing Electronic Health Record (EHR) platforms, creating seamless data flow between patient onboarding and claims processing.
The AI agents maintain comprehensive audit trails while ensuring HIPAA compliance through advanced encryption and access controls.
Intelligent Patient Onboarding Flow
AI agents are changing how patient onboarding works by handling many tasks that used to take up a lot of staff time.
For example, when a patient books an appointment, the system automatically checks their insurance coverage.
It can also tell if there’s a co-payment involved or if the treatment needs pre-approval from the insurer. By doing this upfront, patients are less likely to face last-minute issues during check-in, and staff aren’t stuck making endless phone calls to verify coverage.
Another smart feature is how AI fills out forms. Using natural language processing, the system can understand what patients write or say and then pull the right details to complete forms across different hospital systems.
It even compares the new info with older records or insurance databases, flagging anything that doesn’t match so staff can double-check it. This cuts down form-filling time by 75% and keeps errors to a minimum.
Scheduling also becomes much smoother. The AI looks at doctor availability, insurance rules, and patient preferences all at once.
If an approval is delayed, it can even reschedule the appointment on its own, helping clinics run without unnecessary gaps or missed income.
Lastly, the AI keeps patient records updated with registration, clinical notes, and billing. This means staff don’t have to re-enter data again and again, and hospitals have a complete record ready for audits or reports.
Autonomous Claims Processing Pipeline
AI-powered medical coding represents a significant advancement over traditional manual processes. The system analyzes clinical documentation in real-time, suggesting appropriate CPT and ICD-10 codes with 99.2% accuracy.
Multimodal AI processes voice notes, handwritten forms, and clinical documentation using advanced RAG architectures to ensure medically accurate code suggestions.
Automated prior authorization requests submit directly to insurance providers through electronic systems, reducing processing time from days to hours.
The AI agents track authorization status and proactively follow up on pending requests, ensuring clinical teams have approval before procedure dates.
Predictive denial prevention analyzes historical claims data to identify patterns that lead to rejections. The system flags high-risk claims for additional review before submission, reducing denial rates by up to 78%.
When denials do occur, intelligent appeals generation creates comprehensive responses based on clinical documentation and insurance policy requirements.
AI Agent Technology and Infrastructure
AI agent technology is rapidly reshaping the healthcare industry by providing a powerful backbone for both administrative and clinical workflows.
For healthcare providers, the integration of AI agents with electronic health records (EHRs) means that manual data entry—a major source of administrative burden—can be dramatically reduced or even eliminated.
Instead of spending hours inputting patient data, healthcare professionals can rely on AI agents to automatically extract, validate, and update information from medical history, lab reports, and patient interactions.
This seamless automation not only streamlines data entry but also ensures that patient records are always up to date and accurate, supporting better clinical decision making. AI agents can analyze vast amounts of patient data in real time, using predictive modeling analysis to identify health risks and suggest personalized treatment plans tailored to each individual’s unique needs.
By leveraging natural language processing, these systems can understand and respond to human language requests, making it easier for both patients and staff to interact with healthcare systems.
The result is a significant enhancement in patient care and patient satisfaction. Healthcare professionals are freed from repetitive administrative tasks, allowing them to focus on delivering high quality patient care.
At the same time, patients benefit from more personalized treatment and faster, more accurate service. As AI agents continue to evolve, their ability to support both administrative and clinical workflows will be central to improving health outcomes and operational efficiency across the healthcare industry.
Implementing Guardrails for Healthcare AI: Preventing Hallucinations in Critical Workflows
AI is making big changes in healthcare, but it can also make mistakes. Sometimes it gives wrong answers that sound real. This is known as "hallucination," and it can be dangerous in areas like diagnosis, imaging, or treatment advice.
To avoid this, new rules are coming in. In 2024, the FDA shared fresh guidance on how AI in healthcare should work. It asks for clear testing, regular updates, and proof that the AI works in real-world situations. CMS is also setting rules for when AI tools will get paid for by insurance. If an AI tool can't explain how it works or doesn't show results that doctors can trust, it may not be approved for use.
To make AI safer, healthcare systems are:
- Setting confidence levels before using AI results
- Keeping doctors in control of decisions
- Locking AI tools in high-risk areas like ICUs
These steps help make sure AI supports care without putting patients at risk.
Quantified Benefits: Before vs. After Implementation
The transformation from manual to AI-automated healthcare workflows produces measurable improvements across all operational metrics. Real-world implementations demonstrate consistent results across different hospital sizes and specialties.
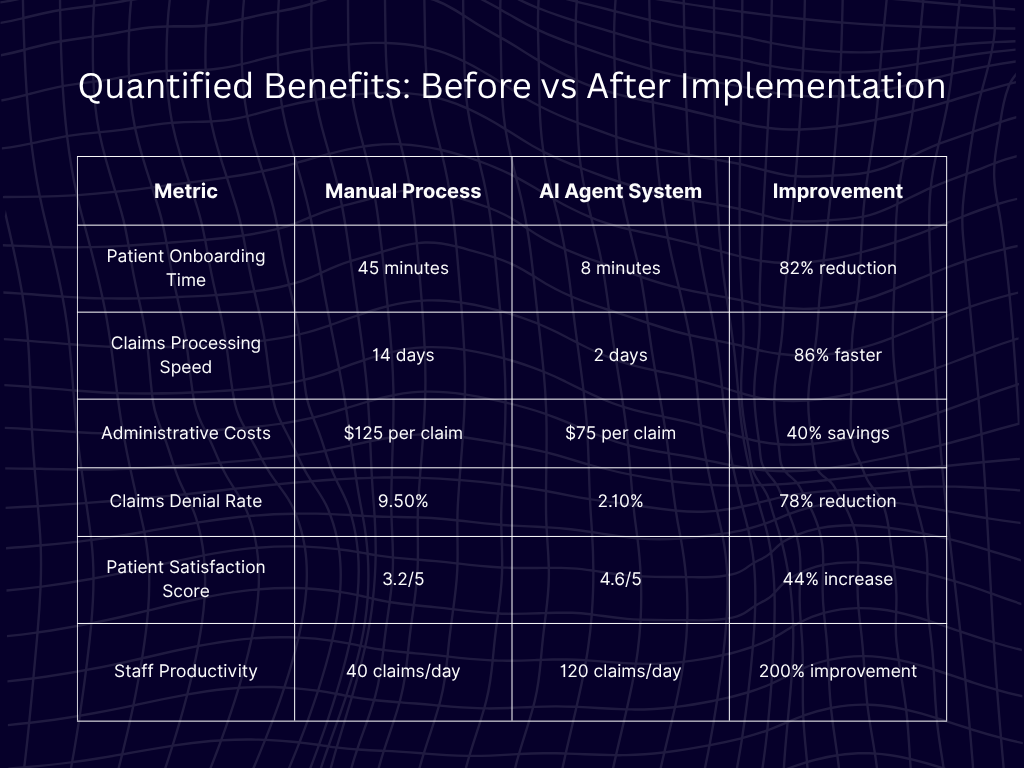
These improvements compound over time as AI agents learn from each interaction. Machine learning algorithms identify optimization opportunities that human administrators might miss, continuously refining workflows to achieve peak efficiency.
Pro Tip: Establish baseline metrics before implementation to demonstrate ROI clearly. Track both quantitative measures (processing time, error rates) and qualitative indicators (staff satisfaction, patient feedback) for comprehensive impact assessment.
Real-World Success: Metro Health System Transformation
Metro Health System, an 850-bed hospital network, implemented AI agents across their revenue cycle operations in early 2024.
The transformation began with a pilot program in their largest facility's emergency department, where patient volumes and complexity created ideal testing conditions.
Within 90 days, patient wait times decreased by 85%, from an average of 52 minutes to under 8 minutes. The AI agents in healthcare administration processed insurance verification automatically while patients completed intake forms, ensuring seamless transitions to clinical care.
Staff reported 95% satisfaction improvement, citing reduced stress and increased time for patient interaction.
The financial impact exceeded projections, with $2.8 million in annual administrative cost savings. Claims processing efficiency improved dramatically, with the denial rate dropping from 11.2% to 2.4%.
The system achieved full ROI within six months, ahead of the projected 8-month timeline.
Measuring Success and Evaluating Effectiveness
To ensure that AI agents are delivering on their promise of better health outcomes and improved patient care, healthcare providers must adopt a data-driven approach to measuring success.
Key performance indicators (KPIs) such as patient satisfaction, patient outcomes, and operational efficiency provide a clear picture of how AI agents are impacting the organization.
By analyzing data from AI agent interactions, healthcare organizations can pinpoint areas for improvement and fine-tune system performance.
This ongoing evaluation helps reduce diagnostic errors, enhance clinical decision making, and boost patient engagement—all of which contribute to higher care quality and better patient outcomes.
Seamless integration with existing healthcare infrastructure is essential, enabling real-time data exchange and supporting informed clinical decisions.
Ultimately, the effectiveness of AI agents is reflected in both quantitative and qualitative improvements: lower costs, fewer administrative burdens, and a more positive patient experience.
As healthcare organizations continue to leverage AI agent technology, they can expect to see not only operational gains but also a measurable impact on the quality of care they provide.
Implementation Roadmap: Your 90-Day Journey
Successful AI agents in healthcare administration implementation follows a structured approach that minimizes disruption while maximizing adoption.
The 90-day timeline allows for thorough testing and staff training while delivering quick wins that build organizational momentum.
Phase 1: Assessment & Setup (Days 1-30)
Current workflow audit identifies specific pain points and quantifies baseline performance metrics. This assessment includes staff interviews, process mapping, and data analysis to understand existing inefficiencies.
The audit reveals integration requirements and potential resistance points that could impact implementation success.
AI agent configuration begins with EHR integration setup and initial rule engine programming. Technical teams establish secure connections between systems while configuring user permissions and access controls.
HIPAA compliance verification ensures all data handling meets regulatory requirements.
Staff training and change management preparation involves creating training materials, identifying champion users, and developing communication strategies. Early engagement helps address concerns and builds enthusiasm for the upcoming changes.
Phase 2: Pilot Launch (Days 31-60)
Department-specific agent deployment starts with the highest-impact area, typically emergency departments or high-volume specialty clinics. Limited scope allows for intensive monitoring and rapid iteration based on real-world performance.
Real-time monitoring tracks system performance, user adoption rates, and initial outcome metrics. Daily check-ins with staff identify issues early while capturing improvement suggestions.
Technical teams make adjustments based on actual usage patterns rather than theoretical scenarios.
Initial performance metric tracking establishes early ROI indicators and identifies optimization opportunities. Weekly reports demonstrate progress to stakeholders while highlighting areas requiring additional attention.
Phase 3: Full Deployment (Days 61-90)
Hospital-wide rollout expands successful pilot configurations across all departments. Lessons learned during the pilot phase inform scaling strategies and help avoid common implementation pitfalls. Staff confidence from pilot success facilitates broader adoption.
Advanced analytics implementation provides deeper insights into workflow optimization opportunities. Predictive analytics identify trends that enable proactive improvements rather than reactive fixes.
Dashboard reporting keeps leadership informed about ongoing performance improvements.
Continuous improvement protocols establish regular review cycles and optimization procedures. Monthly performance reviews ensure the system continues delivering expected benefits while identifying new automation opportunities.
Addressing Executive Concerns: Your AI Agent FAQ
Healthcare executives consistently raise specific concerns about AI agent implementation. Addressing these concerns directly helps build confidence and accelerate decision-making processes.
"How do we ensure HIPAA compliance with AI agents?"
Built-in PII data masking automatically encrypts sensitive patient information while maintaining workflow functionality. All data transmission uses end-to-end encryption with regularly updated security protocols.
SOC 2 Type II certified infrastructure ensures enterprise-grade security standards.
Comprehensive audit trails track every data access and modification, creating complete documentation for compliance reviews. Role-based access controls limit information visibility to authorized personnel only. Regular security assessments and penetration testing validate ongoing protection effectiveness.
"What's the real ROI timeline for healthcare AI agents?"
Break-even typically occurs within 4-6 months, driven primarily by reduced administrative labor costs and improved claims processing efficiency.
Average 3.2x ROI within the first year reflects both direct cost savings and indirect benefits like improved patient satisfaction and staff retention.
Ongoing operational savings of 25-40% compound annually as AI agents learn and optimize performance. Additional benefits include reduced compliance risk, improved data accuracy, and enhanced reporting capabilities that support strategic decision-making.
"Can AI agents integrate with our existing EHR system?"
Over 100 pre-built healthcare integrations support major EHR platforms without custom development.
Epic, Cerner, and Athenahealth native compatibility ensures seamless data flow and user experience consistency. API-first architecture accommodates custom connections for specialized systems or unique workflow requirements.
Integration typically requires 2-4 weeks for standard configurations, with complex customizations extending timelines modestly. Technical support teams provide implementation assistance and ongoing maintenance to ensure optimal performance.
Pro Tip: Request EHR compatibility verification before beginning vendor evaluation. Seamless integration significantly impacts user adoption and ROI achievement timelines.
The Future of Healthcare Operations is Here
Healthcare organizations implementing AI agents for patient onboarding and claims processing achieve remarkable results: 40% cost reduction, 85% faster processing times, and significantly improved patient satisfaction.
The benefits of using AI agents go far beyond just saving time and reducing paperwork. Hospitals that lower their administrative costs with AI can put those savings to better use such as upgrading medical equipment, launching new clinical programs, or offering more training and support for their staff.
When patients notice shorter wait times, smoother check-ins, and fewer billing issues, their satisfaction naturally goes up. That often leads to higher quality ratings for the hospital and more referrals from happy patients.
As more healthcare organizations see how AI improves both operations and patient experience, adoption will pick up speed. Hospitals that start early gain an edge that’s hard for others to catch up with.
At this point, it’s no longer about deciding if AI should be part of the system. The real challenge is figuring out how fast hospitals can put it to work and get results without losing momentum.
Experience the Transformation
Still watching nurses drown in paperwork while patients wait? If that sounds familiar, you don’t have to keep doing things this way.
Ampcome’s AI agents are built to handle the repetitive tasks that drain your staff’s time and energy. Want to see exactly how this could work in your hospital?
In a one-on-one demo, our specialists will map our AI solutions directly whether it’s intake delays, claim denials, or endless data entry. You’ll walk away with a clear plan tailored to your current workflow and real timelines for getting started.
Book your personalized walkthrough at ampcome and see how much your hospital could change in the next 30 days.

Transform Your Business With Agentic Automation
Agentic automation is the rising star posied to overtake RPA and bring about a new wave of intelligent automation. Explore the core concepts of agentic automation, how it works, real-life examples and strategies for a successful implementation in this ebook.
More insights
Discover the latest trends, best practices, and expert opinions that can reshape your perspective
Contact us